South Dakota lags behind the rest of the nation in vaccinating children and youths against the Human Papillomavirus, the most common sexually transmitted disease in America that can cause a range of potentially fatal cancers.
HPV can exist without symptoms and is a leading cause of throat cancer in men and cervical cancer in women, but it is almost entirely preventable through vaccination before someone becomes sexually active. The virus is often spread through intercourse and oral sex but can also transfer through kissing in rare cases.
Federal health data show that South Dakota ranked 41st in the nation in the rate of boys ages 13-15 who are vaccinated against HPV, and 31st in vaccination of girls in that age group in 2016.
The rates have improved since then due to an aggressive education and prevention campaign, yet more than half of adolescents in South Dakota remain unvaccinated.
From 2001 to 2014 in South Dakota, more than 4,700 cases of cancer were likely tied to infections from HPV, leading to an estimated 866 deaths.
Six types of cancer are believed to be related to HPV infection. The virus is responsible for more than 34,000 cases of cancer in the U.S. each year, according to the federal Centers for Disease Control and Prevention.
More than 90% of those cancers could have been prevented by vaccination against HPV, experts say. The HPV vaccine, Gardasil, has been so effective in Australia that the country is on track to virtually eliminate cervical cancer within 20 years, according to a study published in October 2018 in The Lancet, a public health journal.
South Dakota health and medical professionals are aware of the benefits of the vaccine and are working to educate parents and encourage them to get their children vaccinated.
“This is one of the areas where we can prevent cancer through vaccination with our kids and never have to worry about them having to go through that experience,” said Jill Ireland, a senior health systems manager at the American Cancer Society in Sioux Falls.
In 2015 in South Dakota, only 32% of girls and 22% of boys ages 13 to 17 had completed the vaccination dosing regimen, well below the national average of 42% for girls and 28% for boys in that age range, according to the state health department.
After recent aggressive public health and education campaigns, the overall youth vaccination rate against HPV rose to 44.8% for South Dakota adolescents aged 13-17 in 2017, still below the national average of 48.6% that year. By 2018, about 49.5% of 13 to 17-year-olds in the state were current on the HPV vaccine. Nationally, 51.5% of youths in that age range were current on the vaccine.
Even with recent increases, HPV vaccination rates in South Dakota are well below the goal of the federal Healthy People 2020 objective to have 80% of both genders vaccinated by age 15.
South Dakota’s HPV vaccination rate shortfall is particularly significant among girls and young women. CDC data show only 46.3% of girls aged 13-17 were current on the vaccine. Nationally the rate was 53.7%. The HPV vaccination rate for South Dakota boys, however, was slightly higher than the national average of 32.1% at 33.4%.
Health officials say some parents are reluctant to get their children vaccinated against HPV either due to a lack of knowledge of its importance or because they believe it may be unsafe. The shots are not cheap but are generally covered by insurance.

“It’s a problem for some parents because they feel like if they give it to their kids, they’re giving them the right to become sexually active, which is not the case,” said Anderson, whose own children are vaccinated against HPV. “Some parents see it kind of like a sex shot, like they’re giving their child permission to have sexual intercourse at that point. We look at it as a way to prevent a sexual disease that can cause cancer.”
Potentially devastating; almost entirely preventable
Nearly 80 million Americans — about one in four people — are infected with at least one HPV strain. According to the CDC, about 14 million new HPV infections are reported annually, and overall about nine in 10 of all Americans will become infected with HPV during their lifetimes.
Human Papillomavirus is a group of more than 150 related viruses, most of which are fairly harmless and disappear without medical intervention. There are 40 HPV strains that infect mucus membranes and can be spread through any type of sexual contact. Of those, 12 are considered high-risk. Two strains of HPV, types 16 and 18, cause nearly roughly 90% of HPV-related cancers. The newest HPV vaccine, Gardasil 9, protects against both type 16 and type 18 HPV as well as seven other high-risk strains of the virus.
Most people will never know that they were infected by HPV, even if it is one of the high-risk strains. Between 80 and 90 percent of people will be able to fight off the virus on their own. Some people will develop genital warts due to HPV but, for the most part, there are few obvious signs of infection. Serious complications from an HPV infection such as throat or cervical cancer may not appear for years or decades after a person’s first exposure to the disease.
One problem is that there is no way to tell who will be able to fight off HPV and who will not, said Dr. Archana Chatterjee, who chairs the pediatrics department at the Sanford School of Medicine at the University of South Dakota. Not getting the vaccine is a big risk, she said.
“This is a role of the dice to say ‘I’m just going to take my chances of not getting cancer’,” Chatterjee said.

Alysia Juhl was 21 in 2003 when she was told that she was part of the 10 to 20 percent of people who will develop cancer due to HPV. She was a new mother when her doctor found HPV-related cancer cells on her cervix during a post-pregnancy checkup.
“Being a single mom at the time, (the diagnosis) was really tough emotionally,” Juhl said.
She ended up needing a Loop Electrosurgical Excision Procedure, which uses an electrical current in a wire loop to remove abnormal cells from the cervix. The procedure worked and, Juhl said, no more cancer has been found. But her experience with HPV-related cancer wasn’t over.
Years later, Juhl’s husband found a mass on his body that turned out to be a cancerous tumor. The cancer was determined to be HPV-related, though not of the same type that Juhl had been diagnosed with. Multiple surgeries were needed to rid Juhl’s husband of the tumor.
“Luckily, they got everything but the healing process was very difficult,” Juhl said.
Then, in January 2017, Juhl’s then 54-year-old father was diagnosed with cancer of the tonsils. Once again, the cancer was found to be HPV-related. By the end of that month, a feeding tube had been placed in the man’s abdomen and he was starting on a treatment plan that would include 21 radiation treatments, six weeks of chemotherapy and participation in a clinical drug trial as well as two surgeries. Juhl said her father lost more than 100 pounds in addition to his sense of taste and the hearing in one ear.
“It was a very rough time watching him go through all that,” Juhl said.
Now known as a “Vaccination Champion” at the Sanford Health clinic where she works as a nurse, Juhl spends a lot of time talking with patients and parents about the HPV vaccine.
Vaccination of girls against HPV was first recommended in 2006 soon after the FDA approved the first version of Gardasil. South Dakota was one of 25 states that quickly passed legislation aimed at promoting HPV vaccination for girls.
In 2007, the state legislature authorized the Department of Health to spend up to $9 million to get up to 44,000 girls vaccinated against HPV both by paying for the vaccine itself and by increasing awareness of the vaccine. At the time, each dose of what was then a three-shot regimen cost about $360 and wasn’t always covered by insurance.
The CDC began recommending the vaccine for both girls and boys aged 11-12 in 2011. The vaccine is most effective when completed at earlier ages and well before a boy or girl is sexually active.
“It’s like putting on your bike helmet before you get on your bike,” said Andrea Polkinghorn, Sanford Health’s immunization strategy leader in Sioux Falls.
Research on the HPV vaccine has shown that younger children also have better immune responses to the vaccine, meaning they need fewer doses to get the full effect. Before the age of 15, youths now only need two doses for the vaccine to be effective. After the age of 15, they need three.
Today, HPV vaccines are covered by nearly all health insurance plans nationwide because it is considered preventive healthcare under the 2009 Affordable Care Act. Children whose parents don’t have health insurance can get the vaccine for free under the federal Vaccines for Children program.
Despite the HPV vaccine being offered at no cost for most children, public health officials continue to struggle to hit their HPV Vaccination goals.
“This is a fantastic opportunity to prevent cancer … this is just crazy not to utilize every tool we have to prevent these serious types of cancer,” Chatterjee said.
Despite clear benefits, fear persists
South Dakota’s recent efforts to battle the spread of HPV and increase vaccination rates have included making grants to local agencies and medical practices. Those efforts are bearing fruit.
In June 2018, the state issued a grant of roughly $14,000 to Black Hills Pediatrics to undergo an HPV education and prevention effort in the Rapid City area. During a yearlong effort that ended in May 2019, the pediatric office with eight doctors intensified its efforts to notify parents about the need for HPV vaccinations and to encourage them to have their children get the shots.
As part of the program, the practice encouraged all parents of all patients, regardless of the primary reason for their office visit, to get vaccinated against HPV. Furthermore, the practice used text messages, automated phone calls and messaging by office staff to prompt clients to visit the office to get their initial and follow-up vaccine shots.
Overall, more than 4,100 client reminders were issued and nearly 1,500 doses of the vaccine were administered during the yearlong program, a 13% increase in vaccinations over the previous year. That momentum has continued since the grant period ended, said Dr. Anderson, a pediatrician at the clinic.
“We approach parents of all our 11-year-olds, and also check at every visit to see if they have had all their vaccines,” Anderson said. “If they haven’t, we remind them that it’s still available.”
Still, at least part of the problem of low vaccination rates is due to a lack of awareness about why the vaccine is so important, said Andrea Polkinghorn, immunization strategy leader for Sanford Health in Sioux Falls.
"This is a fantastic opportunity to prevent cancer … this is just crazy not to utilize every tool we have to prevent these serious types of cancer." -- Dr. Archana Chatterjee, chair of the pediatrics department at the Sanford Medical School at the University of South Dakota
According to a study published by researchers at Johns Hopkins University in October 2018, 22% of boys’ parents and 20% of girls’ parents said they didn’t know why their child needed the vaccine. Safety concerns were the second most common reason parents cited for not giving their children the HPV vaccine.
One persistent myth about the HPV vaccine is that it is primarily for girls and women, Polkinghorn said. But, according to a 2015 CDC study, men have actually experienced a higher rate of HPV-related mouth and throat cancers than the rates at which women have experienced HPV-related cervical cancer. In one high profile case, actor Michael Douglas, who survived a battle with throat cancer in 2010, acknowledged publicly in 2013 that his cancer was caused by an HPV infection that resulted from oral sex.
“(The vaccine) is really important for males,” Polkinghorn said.
Safety concerns were the second most common reason parents cited for not giving their children the HPV vaccine, Johns Hopkins study said. Roughly 22% of girls’ parents and 14% of boys parents said they weren’t convinced the vaccine was safe, according to the study.
There is no good evidence that the vaccine is unsafe, said Chatterjee. She helped manage the vaccine’s clinical trials while working at Creighton University in Omaha during the early 2000s.
The most common scientifically verifiable side effects of Gardasil 9 include headaches and irritation at the injection site. Slight fevers, nausea, joint and muscle pain also are listed as potential side effects by the CDC. But beyond minor irritation, Chatterjee said, there are few verifiable concerns with the vaccine.
“A lot of the other things you see on the internet aren’t true; those are simply scientifically unproven,” she said.
Vaccines undergo a rigorous testing regime before they can be sold in the U.S., Chatterjee said. Once vaccines are approved, they are tested and monitored even more thoroughly by professional organizations such as the American College of Pediatricians and the U.S. government.
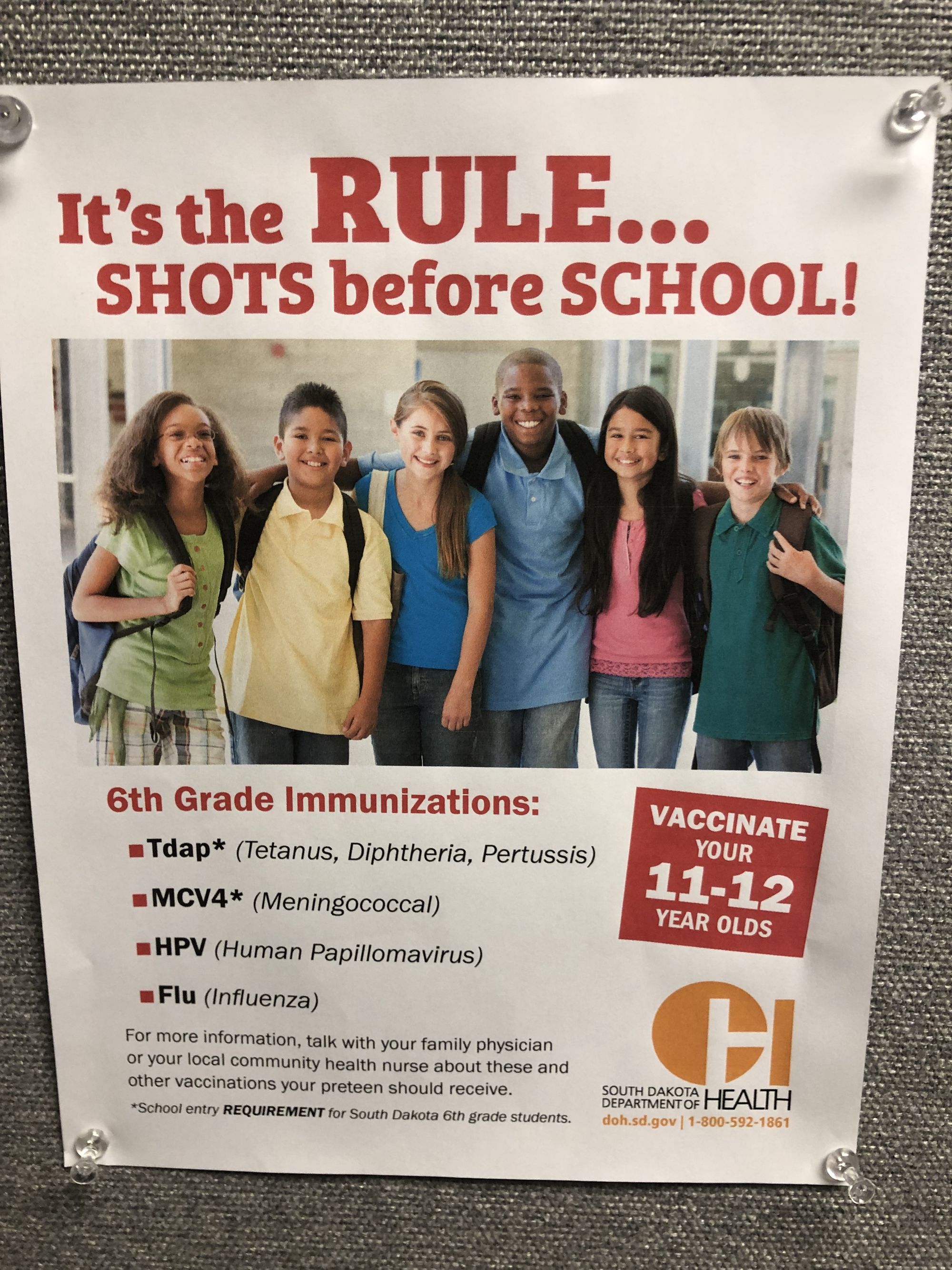
Another problem health officials have run into is that the HPV vaccine often isn’t seen as routine. Unlike other vaccines for such diseases as meningitis, tetanus, diphtheria and pertussis, South Dakota schools don’t require students to get the HPV vaccine before they can go to middle school. Polkinghorn said many of Sanford’s efforts to improve vaccination rates have focused on changing the way providers present the HPV vaccine to parents.
“A lot of it is, because we know the vaccine is safe and that it is effective and that it is recommended that we’re offering it in the same way, on the same day that we offer the other vaccines that are due,” Polkinghorn said.
The Johns Hopkins study also found that about 10% of parents worried their child would become more sexually active after getting the HPV vaccine. This, too, is a concern that hasn’t been borne out by science, Chatterjee said. Over the roughly 13 years that the HPV vaccine has been available in the U.S., teen sexual activity has actually decreased, CDC data show.
There is no question as to whether the benefits of HPV vaccination outweigh the risks, Chatterjee said. One of the first patients Chatterjee worked with was a mother of five in her late 20s who was dying of cervical cancer. The condition had progressed so far that muscles in the patient’s pelvic region had stopped working and bodily wastes were being removed surgically.
“That is something that has stayed with me, that look of sheer fear and anguish on her face, knowing that she was going to die and wondering who would take care of her children,” Chatterjee said. “It gives me great joy in have had a small part in developing this vaccine.”



